Introduction
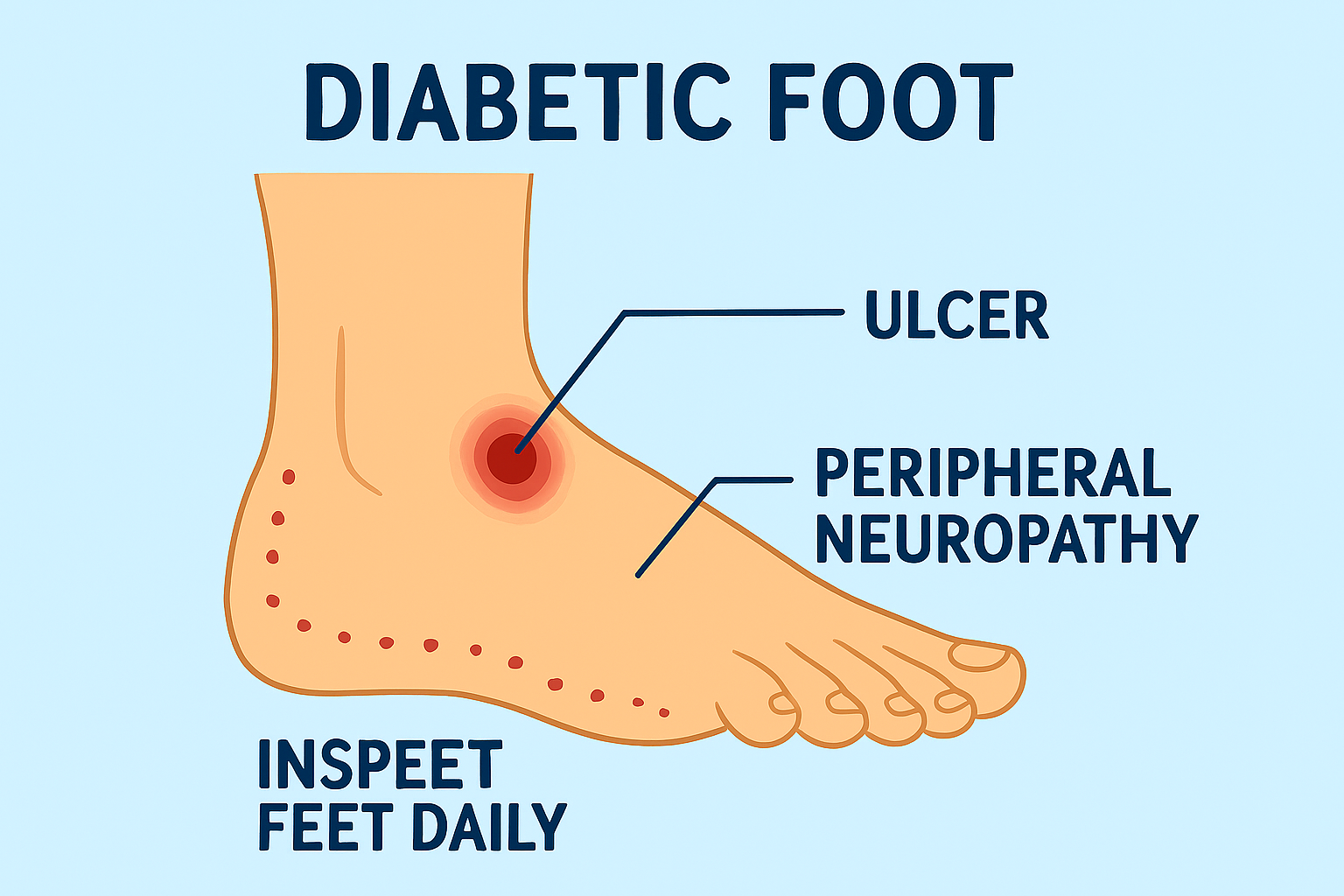
One of the most serious and common complications of diabetes is diabetic foot. Poor circulation, delayed wound healing, and chronic nerve damage are the causes. It can result in infections and, in extreme situations, amputations if left untreated. Patients can take preventative measures and seek prompt care by being aware of this condition.
What Is Diabetic Foot?
Diabetic foot is one of the most often disregarded consequences of having diabetes, which necessitates daily care. This disorder arises when persistently elevated blood sugar damages your blood vessels and nerves, resulting in severe foot issues. Diabetic foot can result in ulcers, infections, and even amputations if treatment is not received. Let’s simplify and make sense of everything you need to know.
The term “diabetic foot” describes a collection of foot disorders that affect individuals with diabetes; these disorders typically include infections, foot ulcers, poor blood flow, and nerve damage (neuropathy). It is one of the main causes of hospital care for people with diabetes.
Medical Expertise: How Diabetes Affects the Feet
Nerve Damage (Diabetic Neuropathy)
Nerves are damaged by high blood sugar, particularly in the legs and feet.
This leads to :
- numbness
- Tingling
- Absence of pain perception
Patients might not be aware of burns, cuts, or other injuries as a result.
Poor Blood Circulation (Peripheral Arterial Disease)
Diabetes causes blood vessels to narrow, which lowers blood flow to the feet.
This results in:
- Slow healing
- An higher risk of infection
- Feet that are cold or discolored
Increased Risk of Ulcers and Infections
Unnoticed injuries, pressure, or poorly fitting shoes can all result in foot ulcers.
Even minor wounds can develop into dangerous infections in diabetics.
Real-World Experience: What Patients Commonly Face
From patient cases and clinical observations:
- Until an ulcer develops, many people are unaware they have neuropathy.
- Due to numbness, minor cuts often go unnoticed.
- Without adequate cleaning and offloading, foot ulcers may develop rapidly.
Patients frequently report:
- A feeling of “pins and needles” or burning
- Walking is difficult because of pain
- Dry or thicker skin
- swelling near the foot or ankle
Types of Diabetic Foot Problems
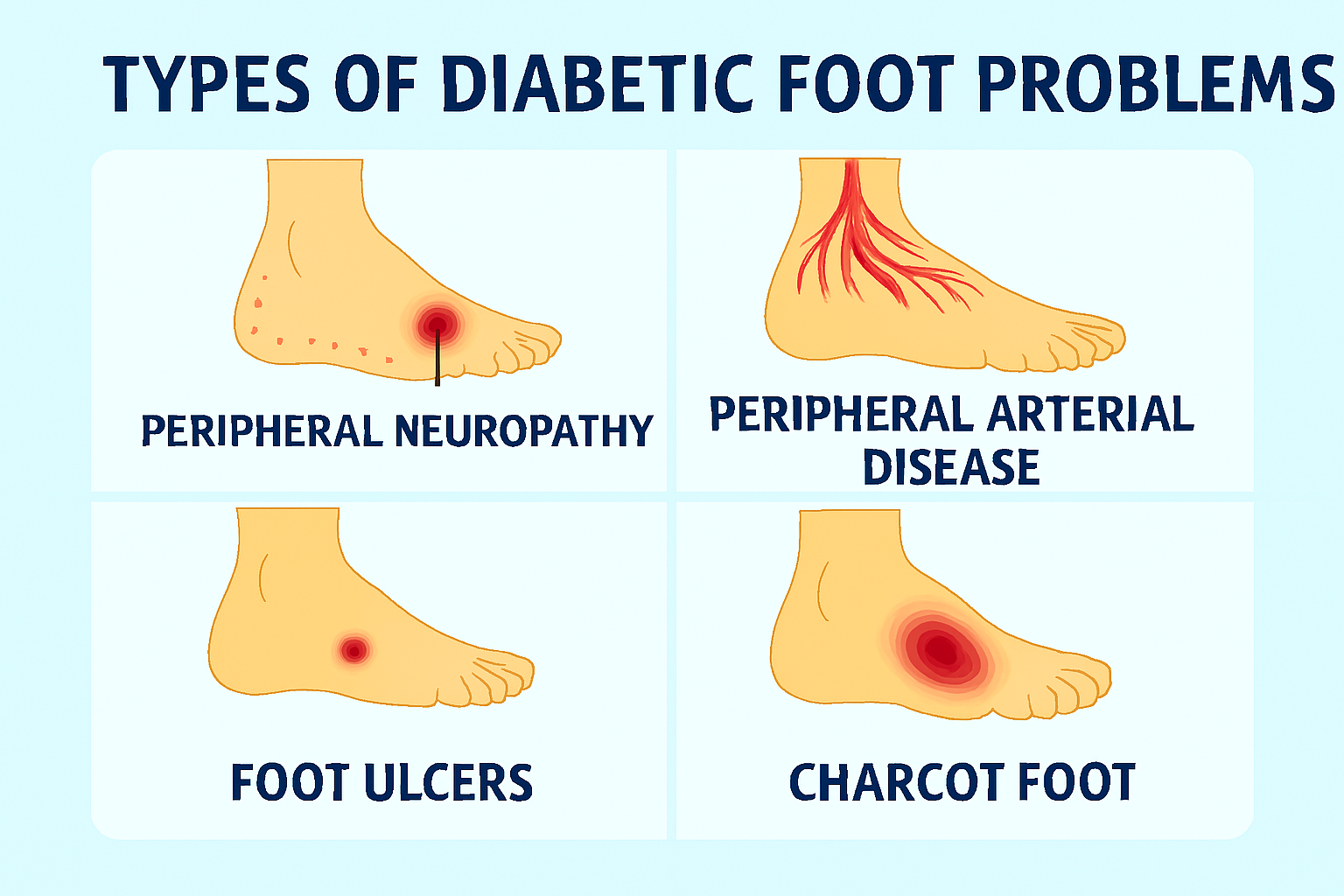
Diabetic Neuropathy
Loss of sensation leading to unnoticed injuries.
Peripheral Arterial Disease (PAD)
Poor blood flow causing slow wound healing.
Foot Ulcers
Open sores commonly found on pressure points like the heel or toes.
Charcot Foot
A rare but severe condition where weakened bones collapse, causing deformity.
Authoritative Medical Insights: Key Warning Signs
seek medical help if you notice:
- Swelling or redness
- Gangrene, or blackened skin
- Open wounds that fail to heal
- A foul smell from the foot
- Pus or fluid discharge
- Blisters or cracks
These symptoms indicate a high-risk situation requiring immediate attention.
Causes and Risk Factors
The main causes of diabetic foot are:
- Uncontrolled diabetes
- Smoking
- High blood pressure or cholesterol
- wearing improper footwear
- Poor hygiene for the feet
- Prolonged diabetes
When taken together, these elements raise the risk of blood vessel and nerve damage.
Diagnosis: How Doctors Check for Diabetic Foot
Physical Examination
Checking sensation, skin condition, wounds, and footwear marks.
Peripheral Nerve Testing
Using tools like:
- Monofilament test
- Vibration tuning fork
Vascular Assessment
To check blood flow:
- Ankle-brachial index (ABI)
- Doppler ultrasound
Imaging
X-ray, MRI, or CT to rule out bone infections or Charcot changes.
Treatment Options Backed by Clinical Practice
Wound Care
- Cleaning
- Debridement (dead tissue removal)
- appropriate dressings
Offloading
reducing pressure using:
- Specialized footwear
- Casts
- Insoles
Medications
- Antibiotics for infections
- Pain relief medicines
- Drugs to improve circulation
Surgical Treatment
Required in severe cases for:
- Removing infected tissue
- Correcting deformities
- Restoring blood flow
Preventive Steps to Reduce Risk
Prevention plays the most powerful role in diabetic foot care.
Daily Foot Care
- inspect your feet daily.
- Thoroughly wash and dry them.
- Moisturize, except between your toes.
- Carefully trim your nails.
Lifestyle Measures
- Maintain stable blood sugar.
- quit smoking
- Engage in regular exercise
- Control blood pressure and cholesterol
Proper Footwear
- Soft, cushioned shoes
- Avoid tight or ill-fitting shoes
- Prefer diabetic-friendly footwear
Regular Check-Ups
A yearly foot exam is essential — more often if you already have neuropathy.
Living With Diabetic Foot
Managing diabetic foot requires:
- consistent control of sugar
- wearing on protective footwear
- Regular consultations with a diabetic foot specialist
Patients often benefit from:
- Education on foot care
- Support groups
- Physiotherapy for mobility
Conclusion
Although it can be avoided, diabetic foot is a dangerous condition. Complications can be significantly decreased by being aware of the risks, seeing early signs, and taking regular care of your feet. Most diabetic foot issues are manageable with prompt treatment and lifestyle changes.
FAQs
1. Is diabetic foot reversible?
Nerve damage isn’t reversible, but early treatment prevents complications.
2. How long does a diabetic foot ulcer take to heal?
Depending on blood flow and sugar control, healing may take weeks to months.
3. What type of doctor treats diabetic foot?
A diabetic foot specialist, podiatrist, or vascular surgeon.
4. Can diabetic foot be prevented?
Yes — with good sugar control, proper footwear, and regular foot exams.
5. Is diabetic foot dangerous?
Yes. If untreated, it can lead to infections, gangrene, and amputations.


