
Introduction
Nursing Management Imagine strolling barefoot on sand that is dotted with small, jagged rocks. Imagine, now, that you are unable to feel those cuts because diabetes damages your nerves. That is the diabetic foot ulcer’s (DFU) silent threat.
As a physician, I frequently see patients who are unaware that they have a wound until it gets infected. These ulcers can result in severe infections and even amputations if treatment is not received. “The good news?” Most diabetic foot ulcers are preventable or curable with appropriate nurse care and patient attention.
1. Understanding Diabetic Foot Ulcers
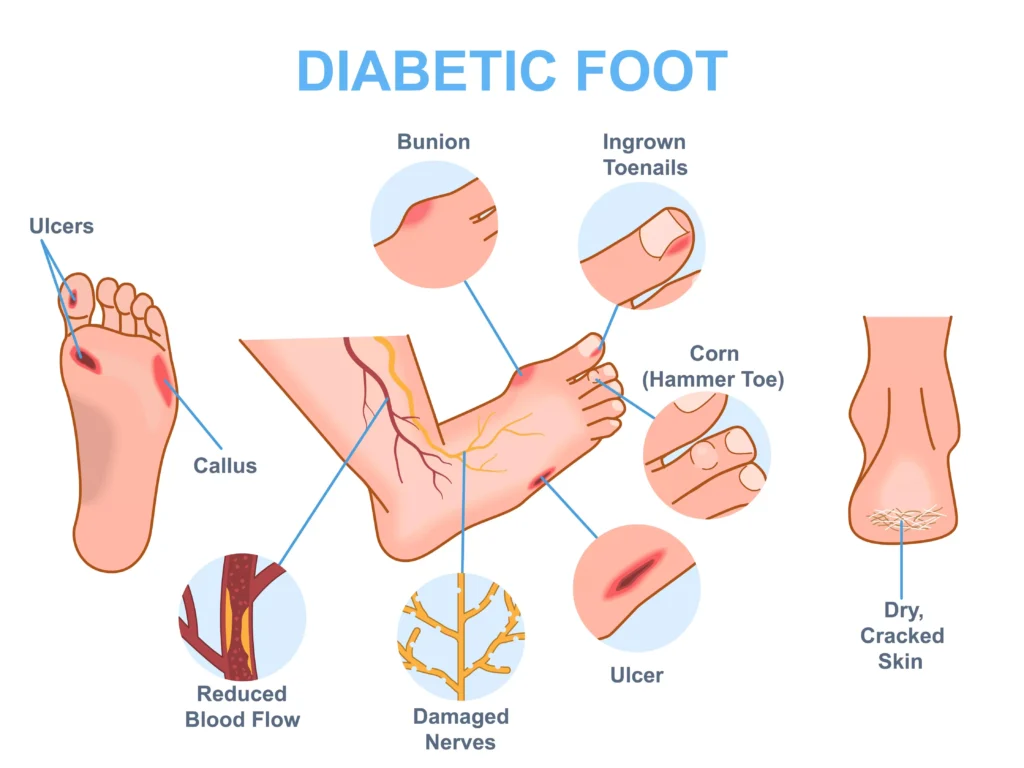
An open wound, typically on the bottom of the foot, caused by inadequate blood supply, nerve loss, or infection in diabetics is known as a diabetic foot ulcer. These ulcers heal far more slowly than a typical wound, and they frequently get worse if left untreated.
Consider the foot to be the building’s foundation. The entire structure deteriorates if foundation fissures are not fixed. In a similar vein, neglecting a diabetic foot ulcer might harm general health.
2. Why Do Diabetic Foot Ulcers Happen?
There are three main reasons:
- Nerve damage (neuropathy):Diabetes damages the nerves, reducing sensation. Patients may not feel injuries.
- Poor circulation:Healing is slowed by decreased blood flow.
- Infections:Wounds with high sugar levels are a haven for germs.
3. Common Signs and Symptoms
- A pain or wound that doesn’t go away
- Warmth, redness, or swelling
- release of an unpleasant odour
- Dead skin is indicated by black tissue
- tingling or numbness in the foot
4. The Role of Nurses in Management
Nurses are the frontline caregivers in diabetic foot management. Their responsibilities include:
- Regularly checking the wound
- Teaching patients how to take care of their feet
- Taking care of injuries and avoiding infections
- directing changes in lifestyle
- Providing emotional assistance
5. Initial Assessment and Diagnosis
Before treatment begins, a nurse or doctor assesses:
- Patient history:length of diabetes, blood sugar regulation, and prior ulcers
- Wound examination:size, depth, and indications of infection
- Vascular check:flow of blood to the feet
- Neurological check:Test of sensation with a tuning fork or monofilament
Planning the appropriate care is aided by this assessment.
6. Wound Care and Dressing Techniques

Proper wound care is the heart of nursing management.
- Cleaning:Saline is used to gently clean wounds.
- Debridement:Skilled specialists remove dead tissue with this procedure.
- Dressing:Certain dressings prevent infection and keep the wound moist.
- Regular monitoring:Changes of clothing are made in accordance with the situation.
A clean, moist wound environment heals faster—like a plant growing well in the right soil.
7. Infection Control and Antibiotics
In diabetic feet, infections proliferate rapidly. Nurses are essential because they:
- Seeing early indications of infection
- Making sure that doctors’ prescription medications are taken on time
- Using sterile dressing methods consistently
- Teaching patients about personal hygiene
Advanced infections can occasionally necessitate surgery or hospitalisation.
8. Pain Management and Comfort Measures
Some people still feel agony, even if many are numb. Nurses handle this by:
- Taking prescription painkillers
- Employing non-pharmacological strategies such as relaxation
- ensuring that the feet are positioned correctly to relieve pressure
Comfort improves healing because stress slows recovery.
9. Patient Education and Self-Care
Half the treatment is patient education. Nurses instruct:
- Inspection of the feet every day
- Using warm water to wash your feet and then carefully drying them
- Don’t put moisturiser between your toes.
- Carefully cutting nails
- Steer clear of barefoot walking
When patients take charge, recurrence rates drop significantly.
10. Importance of Footwear and Offloading
The right shoes are like armor for the feet.
- It is recommended that patients wear comfortable, well-fitting shoes.
- Offloading devices, such as casts or special shoes, relieve pressure on the ulcer, promoting healing.
- Nurses assist patients in selecting and appropriately using these tools.
11. Nutrition and Healing
Food is medicine. For healing ulcers, patients need:
Protein: milk, fish, eggs, and pulses
Vitamins & minerals: iron, zinc, and vitamin C
Controlled sugar intake: limiting sugar consumption to stop more harm
Nurses often work with dietitians to guide patients in meal planning.
12. Preventive Nursing Strategies
Here, the adage “prevention is better than cure” is ideal. Nurses concentrate on:
- Frequent examinations of the feet
- Educating people about proper footwear
- Promoting quitting smoking because it damages circulation
- Encouraging effective diabetes management with medication and lifestyle
13. Emotional and Psychological Support
The fight against a diabetic foot ulcer can seem never-ending. Patients frequently experience depression or a loss of confidence. Nurses offer:
- Support for counselling
- Self-care encouragement
- Link to support groups
Healing is not just physical—it’s mental too.
14. Role of Multidisciplinary Team
Managing DFU is a team effort. Apart from nurses, the team includes:
- Doctors:identify and recommend care
- Podiatrists:Podiatrists are experts in feet.
- Physiotherapists:increase range of motion
- Dietitians:provide dietary guidance
- Psychologists:Psychologists should promote mental wellness.
15. Conclusion and Final Thoughts
A diabetic foot ulcer is more than a wound—it’s a warning sign. But with timely nursing care, patient education, and preventive steps, it can be managed effectively.
As a doctor, I believe the partnership between nurses, patients, and doctors is the key. If you or a loved one has diabetes, don’t wait for wounds to appear. Start with simple steps: check your feet daily, wear the right shoes, and keep blood sugar under control.
FAQs
1. What is the initial nursing intervention for a diabetic foot ulcer?
Assessing the wound, blood flow, and feeling is the initial step in choosing the best course of treatment.
2. How frequently should a diabetic foot ulcer’s bandage be changed?
Usually, every one to two days, or as advised by the healthcare professional, it depends on the state of the wound.
3. Is there a cure for diabetic foot ulcers?
Yes, many ulcers heal with timely treatment, but prevention is always better because recurrence is common.
4. What kind of footwear are ideal for people with diabetes?
footwear with cushioned soles that fit nicely and are soft. Never go barefoot and steer clear of shoes that are too tight or pointed.
5. How may diabetic foot ulcers be avoided at home?
Every day, examine your feet, keep yourself clean, wear appropriate footwear, regulate your blood sugar, and get medical help if you notice any wounds.


