Introduction
Foot Ulcer Symptoms open sore or wound that typically develops on the bottom of the foot is called a foot ulcer. It appears when the skin degrades and reveals the underlying tissue as a result of pressure, poor circulation, or nerve damage. This can be particularly harmful for diabetic patients because elevated blood sugar levels raise the risk of infection and slow down healing.
Causes and Risk Factors
Peripheral neuropathy and diabetes
The most common cause of foot ulcers is diabetes. Numbness results from neuropathy, or damage to the nerves caused by high blood sugar. This indicates that patients frequently do not experience pressure points or minor injuries that could develop into ulcers.
Vascular problems and poor circulation
Peripheral artery disease (PAD) reduces blood flow, which hinders the body’s capacity to fight infections and heal wounds.
Foot Deformities and Pressure Points
Ulcers frequently develop in pressure points created by foot abnormalities like hammertoes or bunions.
External Injuries and Infections
If left untreated, even minor cuts or blisters can develop into ulcers, particularly in patients with weakened immune systems.
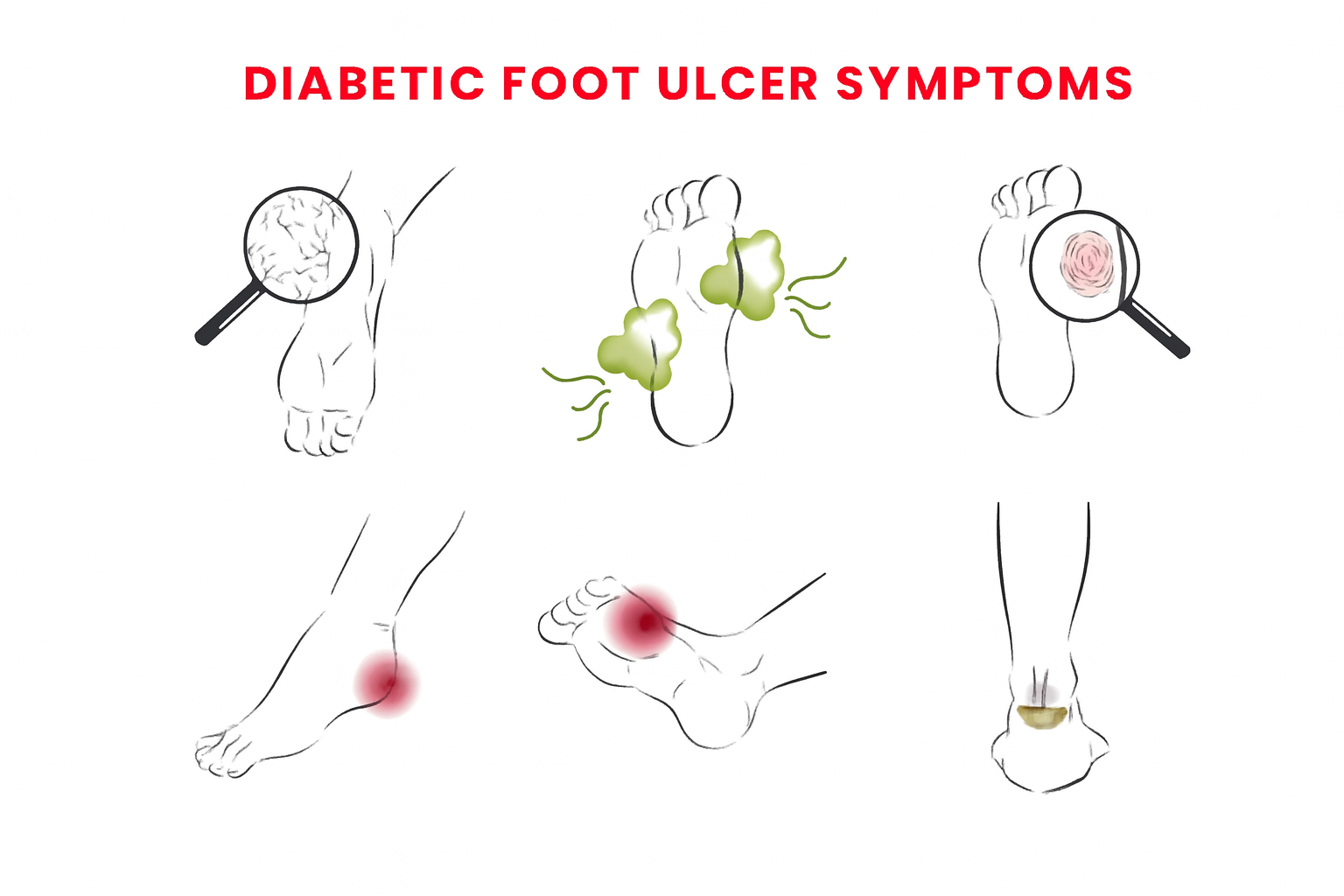
Early Signs and Foot Ulcer Symptoms
Skin Discoloration and Redness
Persistent redness surrounding a specific area, signifying irritation or pressure, is among the initial symptoms.
Sustained Swelling
Ankle or foot swelling indicates an underlying infection or inflammation.
Bad Smell or Emission
A bacterial infection is indicated if a wound drains pus or has an unpleasant odor.
Burning sensation, numbness, or pain
Even as the ulcer gets worse, neuropathy can cause tingling or burning sensations, or, ironically, no pain at all.
Unhealing Blister or Visible Wound
A doctor should always be consulted if a sore doesn’t get better in two weeks.
Calloused or Thickened Skin
Calluses should be carefully treated because they can conceal deep ulcers underneath.
How Doctors Diagnose Foot Ulcers
The first thing that doctors do is physically examine the wound and surrounding tissue. To determine the severity, they might employ wound classification schemes such as the University of Texas or Wagner systems.
To determine whether the infection has progressed to the bone, X-rays or MRI scans may occasionally be prescribed. Blood tests are useful for detecting underlying illnesses like infections or inadequate glucose regulation.
Stages of Foot Ulcers

Stage 1: Damage to the Skin at the Surface
Small patches of openness, flaking, or redness.
Stage 2: Involvement of Deeper Tissue
The ulcer spreads into the subcutaneous tissue or dermis.
Stage 3: Necrosis and Infection
There may be tissue death, pus, and an unpleasant smell.
Stage 4: Bone Exposure or Gangrene
When the ulcer reaches bone or muscle at this point, immediate surgery might be required.
Warning Signs of Infection
Keep an eye out for:
- Warmth or redness around the wound has increased.
- Pus or an unpleasant-smelling discharge.
- Chills, fever, or exhaustion.
You must get medical help right away if any of these happen.
When to See a Doctor
If a foot wound doesn’t heal after more than a week, don’t ignore it. In addition to properly cleaning the wound and prescribing antibiotics or specialty dressings, doctors are able to evaluate the risk of infection.
Treatment Options for Foot Ulcers
Debridement and Cleaning
Debridement is the process by which doctors remove dead tissue in order to encourage healing.
Infection Control and Antibiotics
Antibiotics, whether topical or oral, combat bacterial infections.
Relieving Pressure and Offloading
Casts, special boots, or custom shoes relieve pressure on the wound.
surgical intervention
Surgery might be necessary in extreme situations to remove infected tissue or enhance circulation.
Preventing Foot Ulcers
Foot Inspections Every Day
Every day, look for cuts, blisters, or redness on your feet, especially in the space between your toes.
Wearing the Right Shoes
Put on comfortable, well-fitting shoes to lessen pressure points and friction.
Controlling Blood Sugar and Diabetes
Blood sugar levels that are stable promote healing and lower the risk of infection.
Seeing a podiatrist on a regular basis
Frequent checkups aid in the early detection of changes before ulcers develop.
Lifestyle Tips for Better Foot Health
- Keep up a healthy, vitamin-and mineral-rich diet.
- To increase circulation, stop smoking.
- To improve blood flow, do some light exercise.
- Every day, give your feet a thorough wash and drying.
Aspects of Emotion and Psychology
Mental health can be impacted by having chronic wounds. Patients can manage their stress, anxiety, and fear of ulcers or potential amputations with the aid of counseling or support groups.
Doctor’s Advice for Patients
- Report fresh wounds as soon as possible.
- Never try to treat ulcers on your own.
- Observe the offloading guidelines and take your medication as directed.
- Make sure your feet are dry, clean, and safe.
Conclusion
Particularly in diabetic patients, foot ulcers are a dangerous but avoidable consequence. Early detection of symptoms, like swelling, redness, and wounds that don’t heal, can save both your foot and your life. The majority of ulcers can heal without surgery with the right care, proper hygiene, and ongoing medical supervision.
FAQS
1. What is a foot ulcer’s initial symptom?
Usually, it starts as a minor sore that doesn’t go away or as redness or swelling.
2. Are foot ulcers self-healing?
Most minor ulcers need medical attention to avoid infection.
3. How are foot ulcers treated by medical professionals?
Cleaning, dressing, antibiotics, and offloading pressure are all part of the treatment.
4. Do foot ulcers hurt?
Yes, occasionally, but even in cases of severe ulcers, diabetic neuropathy can cause no pain.
5. If I have diabetes, how can I avoid developing foot ulcers?
The best preventive measures are blood sugar control, appropriate footwear, and daily foot checks.


