Introduction
Diabetic Foot Symptoms affects all areas of your body, particularly your feet, and is not just a problem with blood sugar levels. As a doctor, I have witnessed innumerable instances where basic foot care neglect resulted in serious consequences, including amputation. The first line of defense and prevention is being aware of the symptoms of diabetic foot, from early warning to more severe stages.
Understanding Diabetes and Its Impact on Feet
Blood vessels and nerves are harmed when blood sugar levels remain elevated over time. Your feet are more susceptible to injury and infection as a result of poor circulation and loss of sensation. If a small cut is overlooked, it can quickly become a serious wound.
Why Diabetic Foot Problems Occur
The primary causes are peripheral arterial disease (poor blood flow) and diabetic neuropathy (damage to the nerves). Damage to your nerves stops you from feeling pain, and poor circulation slows the healing process. The combination is ideal for the development of infections, ulcers, and in extreme situations, gangrene.
The Importance of Early Detection
The difference between a full recovery and permanent disability can be determined by early detection. Frequent foot examinations, both at home and at doctor’s appointments, aid in detecting symptoms before they become serious issues.
Common Early Symptoms of Diabetic Foot

Tingling or Numbness
A tingling or “pins and needles” feeling is one of the initial warning indicators. It might begin in your toes and work its way up. High blood sugar damages the small nerves in your feet, which is why this occurs.
Burning Sensation
Particularly at night, some patients complain of a burning or shooting pain. This may indicate peripheral neuropathy, another name for inflammation of the nerves.
Dry or Cracked Skin
Your feet may become dry and cracked if there is damage to the nerves that regulate the sweat glands. Bacteria may be able to enter through these cracks.
Swelling or Redness
Mild redness or swelling could be a sign of infection or inflammation. It is worthy of medical attention, regardless of how minor it may appear.
Moderate Symptoms That Indicate Progression
Persistent Pain or Discomfort
Some diabetics experience persistent pain, which suggests moderate nerve damage, even though many lose sensation.
Calluses or Corns
Pressure points are the cause of these thickened skin patches. They may decompose into ulcers if left untreated.
Slow-Healing Sores
It is a warning sign if a minor cut or blister doesn’t heal in a week. High blood sugar and poor circulation slow the healing of wounds.
Severe Diabetic Foot Conditions
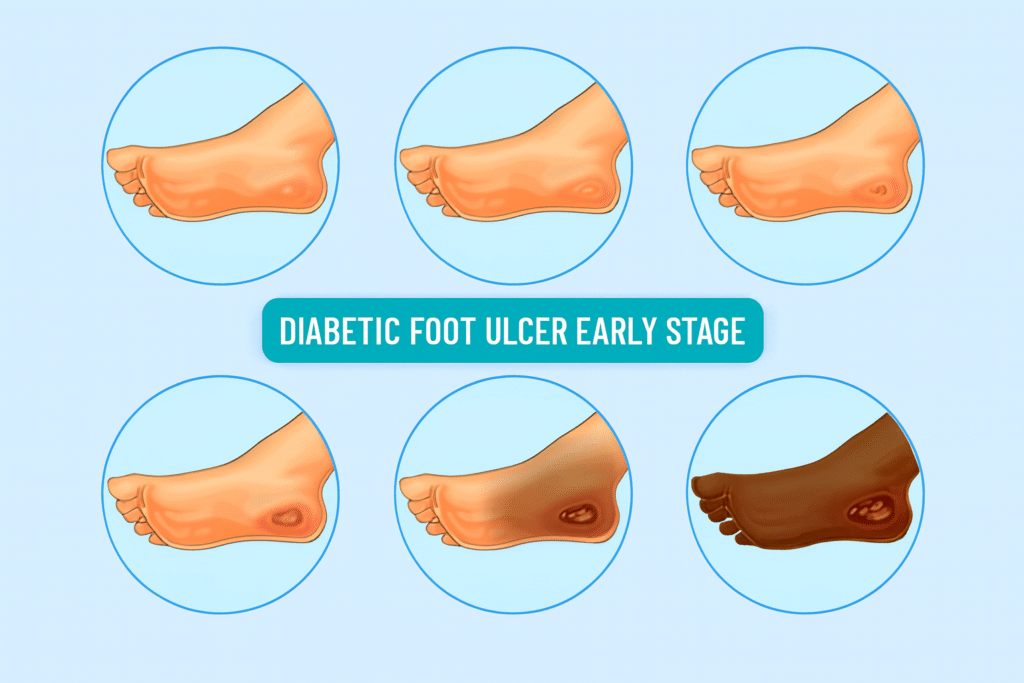
Foot Ulcers
These are open wounds that typically form on pressure points, like the foot’s ball or heel. Among diabetics, ulcers are the most frequent reason for hospitalization.
Infections and Abscesses
Because of weakened immunity, infection spreads swiftly once bacteria get inside through an ulcer or crack. Bones and tissues may be affected by deep infections.
Gangrene
Gangrene occurs when tissues begin to die due to a complete blockage of blood flow. This is an urgent medical situation that calls for surgery right away.
Charcot Foot
a rare but dangerous disorder that causes the structure of the foot to deform as bones weaken and collapse. Because of numbness, it is frequently overlooked.
How to Self-Examine Your Feet
- Use a mirror to examine your feet every day.
- Look for cuts, cracks, or discoloration between the toes.
- Check for edema or morphological changes.
- Check for ingrown edges or infections under the toenails.
Later hospital visits may be avoided with early detection during self-checks.
When to See a Doctor
Consult your doctor immediately if you notice:
- Continuous discomfort or edema
- Open lesions or ulcers
- foul smell coming from a wound
- Skin that is discolored.
- drainage or PUS
Don’t wait for things to get worse. Prompt care saves lives and saves feet.
Diagnosis and Clinical Evaluation
Doctors may use:
- Nerve sensitivity testing using monofilament.
- Doppler ultrasonography to measure blood flow.
- X-rays and wound swabs to look for bone involvement or infections.
These aid in identifying the condition’s severity and stage.
Medical Management and Treatment Options
Antibiotic Therapy
prescribed for infections in accordance with the findings of wound cultures.
Wound Care and Dressings
In addition to promoting healing, sterile, moisture-balanced dressings also help to avoid infection.
Debridement
Recuperation depends on the removal of diseased or dead tissue.
Surgery in Severe Cases
Surgery or even amputation may be required if gangrene or infection spreads to the bone.
Preventive Foot Care for Diabetic Patients
Daily Foot Inspection
Examine your feet daily, especially after taking a bath, to develop the habit.
Proper Foot Hygiene
Apply moisturizer after washing with lukewarm water and making sure everything is completely dry (avoid between toes).
Choosing the Right Footwear
Put on shoes that fit properly and offer injury protection. Even indoors, avoid going barefoot.
Controlling Blood Sugar Levels
The cornerstone of diabetic foot prevention is effective glycemic control. Damage to the nerves and vessels can be avoided with regular monitoring and diet control.
Role of a Doctor in Managing Diabetic Foot
Protecting the limb and the patient’s quality of life is our mission as doctors. We assess, educate, and take early action. Comprehensive management is ensured by multidisciplinary care involving vascular surgeons, endocrinologists, and podiatrists.
Complications If Left Untreated
Neglecting diabetic foot symptoms can lead to:
- persistent infection
- involvement of the bones (osteomyelitis)
- Amputation
- Sepsis, a potentially fatal infection
The best defense is still prevention and early treatment.
Conclusion
Your feet serve as your foundation, so look after them. Symptoms of diabetic foot can be minor at first, but they can have a profound effect. You can live a healthy, active life free from complications with the support of appropriate medical advice, early intervention, and routine examinations.
FAQS
1. What is the initial indication of a diabetic foot condition?
The first symptoms are frequently burning, tingling, or numbness in the feet.
2. How can diabetic foot ulcers be avoided?
Wear appropriate footwear, check your feet every day, and manage your blood sugar.
3. Is it possible to fully cure diabetic foot?
Even though nerve damage cannot be repaired, it can be stopped from getting worse with the right treatment.
4. How frequently should a diabetic see a podiatrist?
At least every three to six months, or right away if you see any infections or wounds.
5. Can diabetic foot cases be prevented by amputation?
Yes, the majority of severe cases can be managed without amputation if identified and treated early.


