
Introduction
One of the most prevalent but avoidable complications among diabetic patients is diabetic foot problems. From a medical professional’s perspective, diabetic foot surgery is a life-saving measure rather than merely a medical procedure. The objective is always the same, whether the patient has severe wounds, poor blood flow, or advanced infections: to save the limb and save the life.
Understanding Diabetic Foot Problems
Why Diabetes Affects the Feet
Over time, diabetes silently damages blood vessels and nerves. Physicians frequently observe:
- Diminished feeling (neuropathy)
- Inadequate circulation
- Slow healing of wounds
The feet are susceptible to infections and ulcers as a result of this combination.
Common Foot Complications in Diabetic Patients
According to medical professionals, the most common complications are:
- ulcers on the feet
- Gangrene
- formation of an abscess
- Osteomyelitis, a bone infection
- Charcot foot and other deformities
Patients frequently require surgery as a result of these problems.
When Surgery Becomes Necessary
Doctors think about surgery when:
- Medication is not effective in healing wounds.
- Infection spreads more deeply
- There is a very limited supply of blood.
- Because of sepsis, there is a risk to life.
Doctor’s Approach to Diabetic Foot Assessment
Detailed Medical History
Doctors begin by comprehending:
- The length of diabetes
- Medicines
- Previous foot issues
- Blood glucose regulation
This sheds light on the potential for healing.
Clinical Examination
Physicians carefully examine:
- Doctors closely inspect:
- Skin color
- Temperature
- Pulses in the feet
- Presence of ulcers
- Signs of infection or deformity
Diagnostic Tests and Imaging
Doctors may request:
- X-raying
- MRI pictures
- Doppler testing
- Blood analyses
These aid in determining the severity of the illness.
Types of Diabetic Foot Surgeries
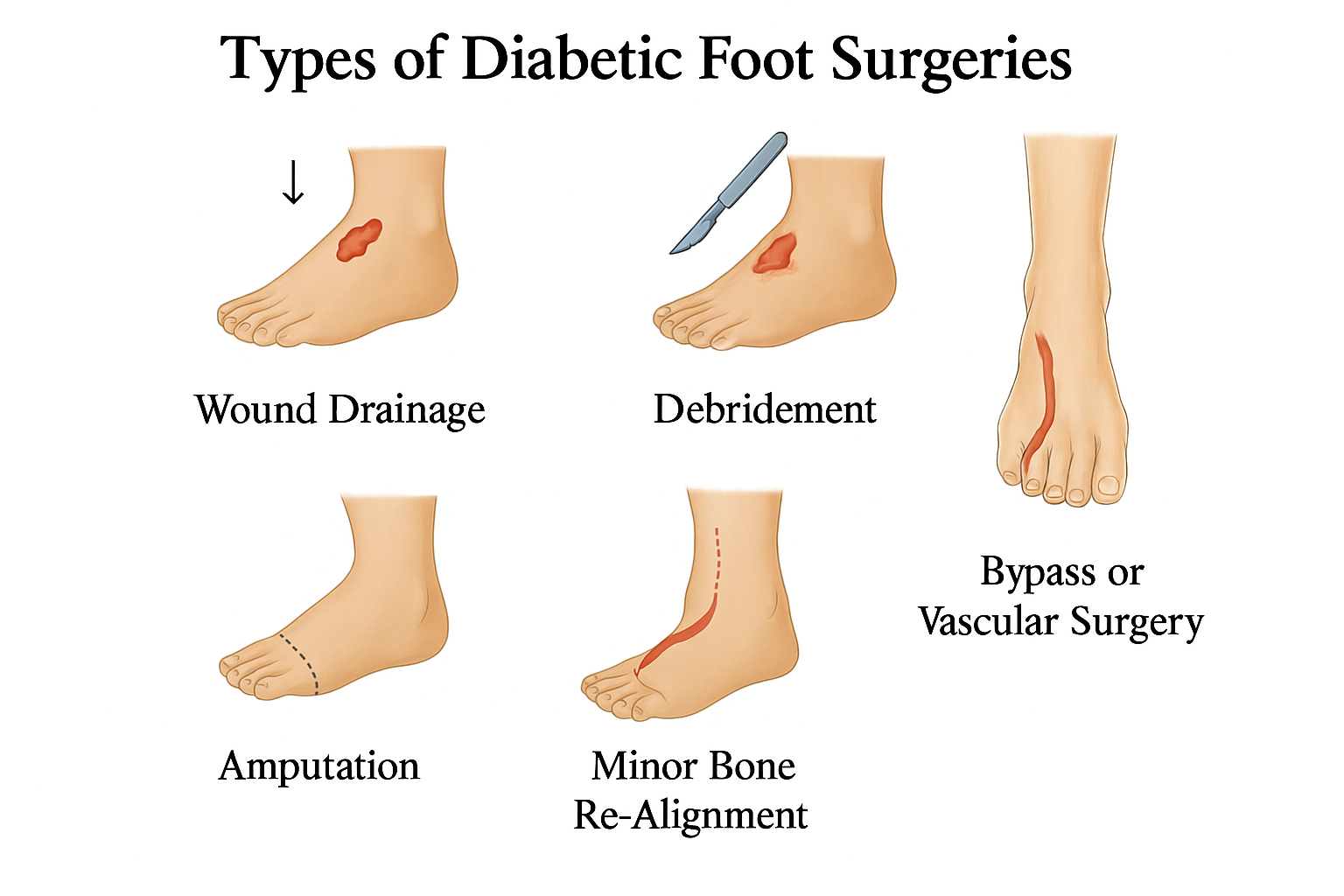
Debridement Surgery
This is the first-line surgical step for most diabetic wounds.
How Doctors Perform Debridement
Infected or dead tissue is extracted to:
- Stop the spread of infection
- Encourage healing
- Boost the area’s blood supply
Physicians employ surgical instruments or sophisticated techniques such as mechanical or enzymatic debridement.
Abscess Drainage
Sometimes infections spread under the skin and form pockets of pus.
Why Abscesses Are Dangerous
If they are not drained, they can rapidly develop into potentially fatal infections. To avoid more issues, surgeons carefully open and clean these pockets.
Bypass or Vascular Surgery
This surgery focuses on improving blood circulation.
Improving Blood Flow to Save the Limb
Physicians may do:
- The Angioplasty
- Grafting bypass
Improved blood flow prevents amputation.
Reconstructive Surgery
Used when deformities cause repeated ulcers.
Correcting Foot Deformities
Examples consist of:
- Lengthening of tendons
- Correction of bones
- Reconstruction of the Charcot foot
Patients who undergo these procedures walk more comfortably and face fewer risks in the future.
Amputation
This is not a doctor’s first choice but sometimes the only safe option.
When It Is the Last Option
Amputation is required when:
- The bone becomes infected.
- Gangrene is the death of tissue.
- The blood supply cannot be replenished.
- Life is in danger.
The goal of doctors is to maintain as much limb length as they can.
Surgical Decision-Making from a Doctor’s Perspective
Evaluating Patient Condition
Doctors assess:
- Blood glucose levels
- Heart wellness
- Renal function
- Level of overall infection
Balancing Risks and Benefits
Surgeons weigh:
- Will the limb be saved by the surgery?
- Will the patient recover appropriately?
- Is it possible to control infection?
Multidisciplinary Team Approach
Doctors collaborate with:
- Endocrinologists
- Vascular surgeons
- Podiatrists
- Experts in infections
Results are improved by this cooperation.
What Doctors Prioritize Before Surgery
Infection Control
Antibiotics and cleaning techniques are used by doctors to lower the bacterial load.
Blood Sugar Stabilization
Strict control is necessary because high blood sugar prevents healing.
Improving Circulation
If circulation is poor, vascular interventions are planned.
Post-Surgery Care: What Doctors Expect from Patients
Wound Care and Dressing
The surgical site needs to be kept clean and covered by bandages.
Offloading and Mobility Restrictions
Doctors recommend:
- Unique footwear
- All-contact casts
- Walking very little
Follow-Up Visits and Monitoring
Regular check-ups help ensure the wound heals properly.
Prevention According to Doctors
Daily Foot Checks
Doctors advise:
- inspecting feet every day
- Examining in between the toes
- Searching for wounds or edema
Choosing the Right Footwear
Avoid tight shoes. Use soft, cushioned footwear.
Managing Diabetes Effectively
Proper diet, medication, and monitoring prevent complications.
Conclusion
Diabetic foot surgery is more than a medical procedure—it is a journey of healing, prevention, and long-term care. From a doctor’s perspective, every effort is made to avoid surgery, but when it becomes necessary, the goal is clear: save the limb and protect the patient’s life. Understanding the surgeon’s viewpoint helps patients appreciate the importance of early detection, proper diabetes management, and timely treatment.
FAQs
1. Why is diabetic foot surgery necessary?
When the limb or life is in danger due to an infection, poor blood flow, or ulcers, it becomes necessary.
2. Is surgery necessary for all diabetic foot wounds?
No, surgery is only necessary for severe or non-healing wounds.
3. How long does it take to recover from diabetic foot surgery?
Blood sugar regulation, circulation, and the type of surgery all affect recovery.
4. Is it possible to avoid diabetic foot issues?
Indeed. Risks are greatly decreased by regular foot care, appropriate footwear, and managed diabete.
5. Is amputation always the last option?
Of course. Amputation is only recommended by doctors when there is no other way to save the limb.


