Introduction
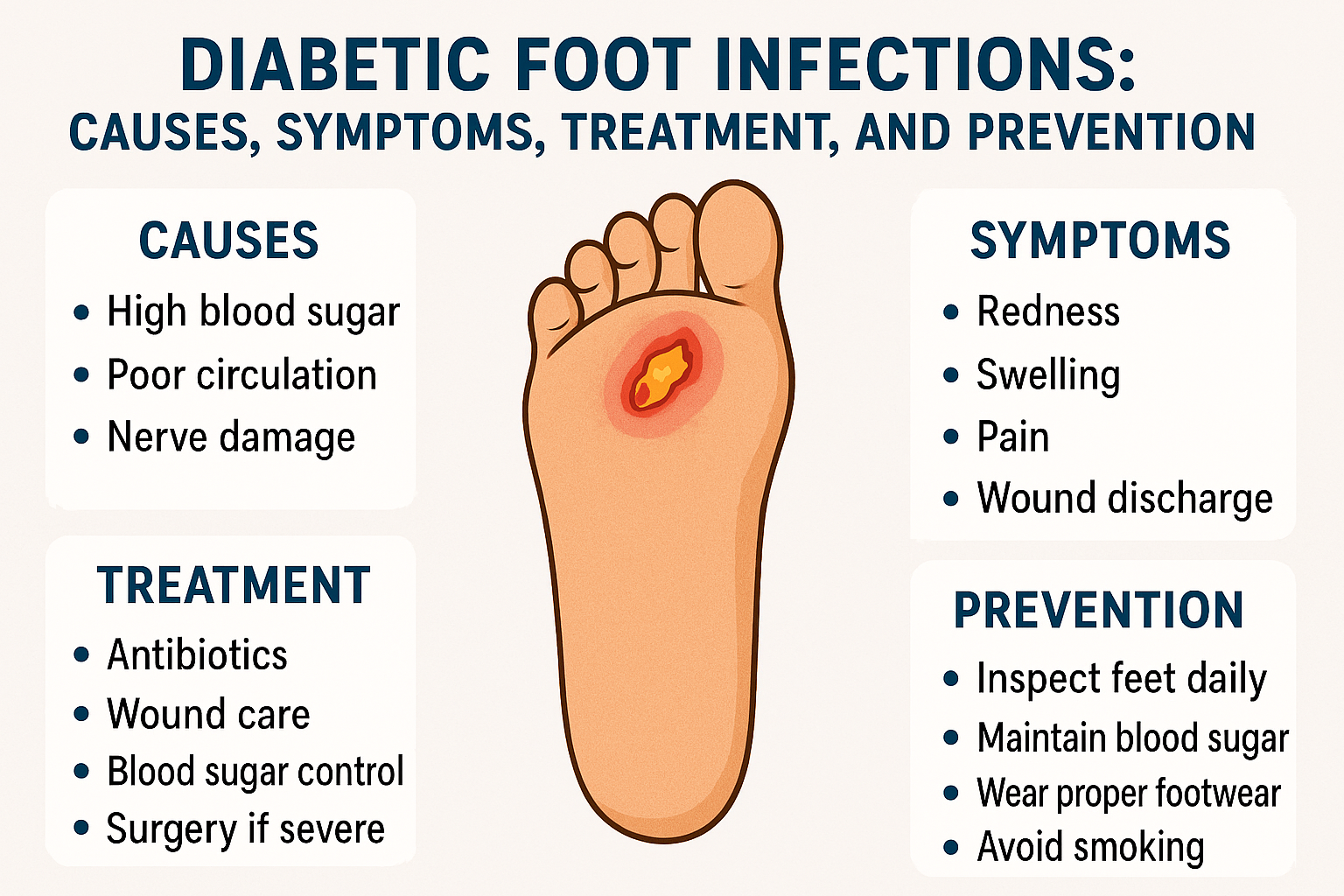
Diabetic foot infections are one of the most serious yet preventable complications of diabetes. Think of them like a small spark that can turn into a wildfire if ignored. What starts as a tiny cut or blister can slowly evolve into a deep infection, threatening not just the foot but sometimes a person’s life. The good news? With the right knowledge, early action, and consistent care, most diabetic foot infections can be avoided or effectively treated.
Understanding Diabetic Foot Infections
What Is a Diabetic Foot Infection?
A diabetic foot infection occurs when bacteria or fungi invade the tissues of the foot in a person with diabetes. These infections usually begin in open wounds, ulcers, or cracks in the skin. Because healing is slower in diabetics, infections get a free pass to grow deeper and wider.
Why Diabetics Are at Higher Risk
Diabetes affects the body like rust affects metal—slowly but surely. High blood sugar damages nerves and blood vessels, reducing sensation and blood flow to the feet. This means injuries go unnoticed and healing takes longer, creating the perfect storm for infections.
How Diabetes Affects Foot Health
Diabetes is a chronic condition that affects how the body processes blood sugar (glucose). Over time, uncontrolled or poorly managed diabetes can lead to several complications—one of the most serious and common being foot problems. Understanding how diabetes affects foot health is essential for prevention, early detection, and long-term well-being.
Role of High Blood Sugar Levels
Persistently high blood sugar weakens the immune system. Imagine trying to fight an enemy with half your army asleep—that’s what your body faces when glucose levels are uncontrolled.
Nerve Damage (Diabetic Neuropathy)
Neuropathy causes numbness, tingling, or complete loss of sensation. A stone in the shoe or a small blister may go unnoticed for days, worsening with every step.
Poor Blood Circulation
Reduced blood flow means less oxygen and nutrients reach the foot. Wounds heal slowly, and infections linger longer than they should.
Consequences of poor circulation
- Delayed wound healing
- Increased risk of infections
- Dry, cracked skin
- Cold or pale feet
Common Causes of Diabetic Foot Infections
Diabetic foot infections are a serious and frequent complication of diabetes. They usually develop due to a combination of nerve damage, poor circulation, and reduced immunity. Understanding the common causes helps in early prevention, timely treatment, and avoidance of severe complications such as gangrene or amputation.
Minor Cuts and Injuries
Even a small nail cut or razor nick can become a serious issue if not cleaned and treated promptly.
Simple injuries such as:
- Cuts from nail trimming
- Blisters from tight shoes
- Cracks in dry skin
Foot Ulcers
Diabetic foot ulcers are open sores that refuse to heal. They’re the most common entry point for infections.
Causes include:
- Repeated pressure
- Improper footwear
- Foot deformities
Once the skin barrier breaks, bacteria can easily enter, leading to infection.
Improper Footwear
Tight shoes, hard soles, or ill-fitting sandals cause friction and pressure points.
- Constant friction
- Pressure sores
- Corns and calluses
These conditions may break the skin and allow infection to develop.
Walking Barefoot Risks
Walking barefoot—even at home—exposes feet to sharp objects, burns, and infections. One step can change everything.
Types of Diabetic Foot Infections
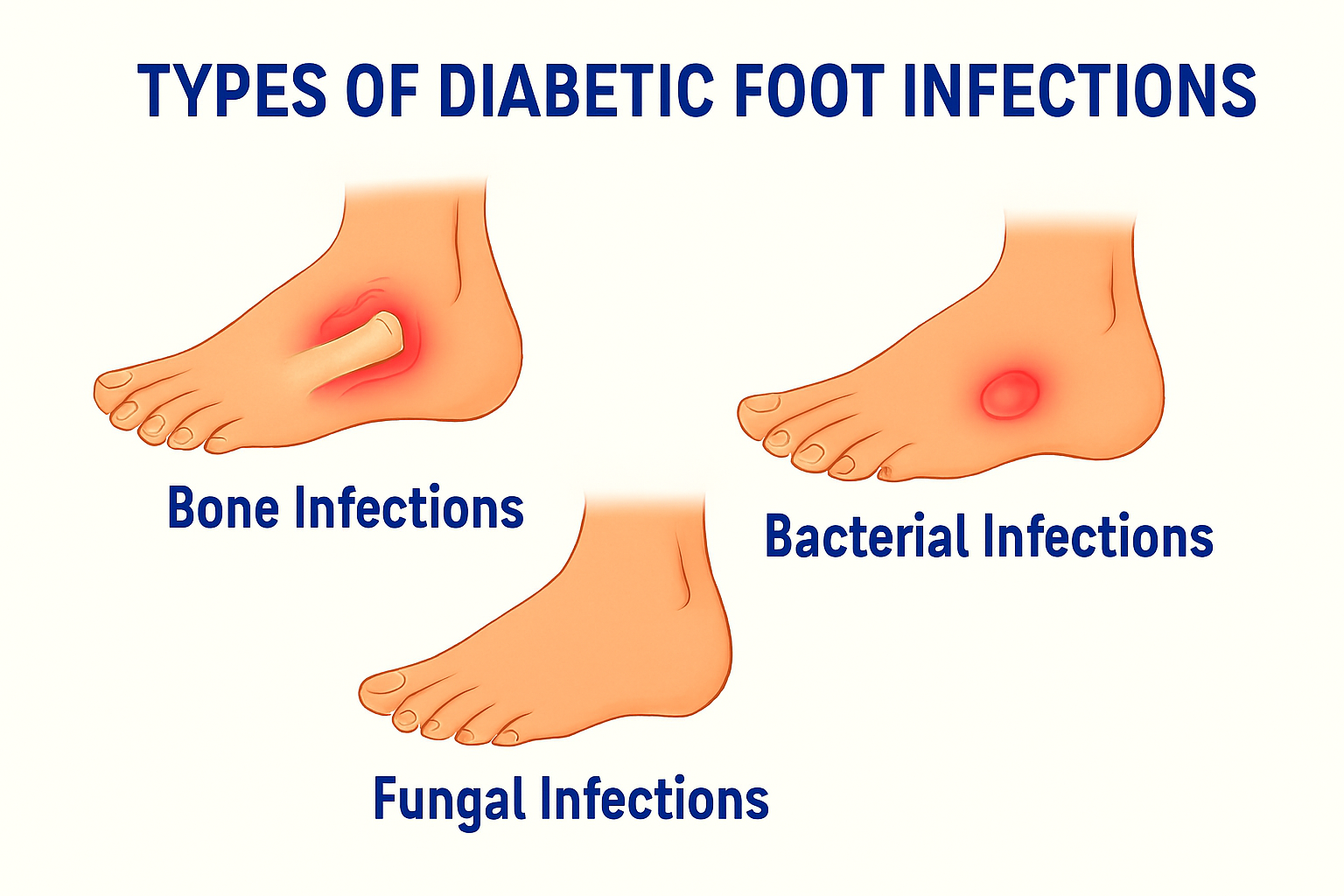
Bacterial Infections
These are the most common and often involve Staphylococcus or Streptococcus bacteria.
Fungal Infections
Athlete’s foot and fungal nail infections create cracks in the skin, allowing bacteria to sneak in.
Bone Infections (Osteomyelitis)
When infections reach the bone, treatment becomes longer and more complex, often requiring surgery.
- Infection of the bone
- Occurs when infection spreads from a chronic ulcer
Features:
- Deep or long-standing ulcer
- Bone exposure
- Persistent infection
Early Warning Signs and Symptoms
Local Symptoms
- Redness
- Swelling
- Warmth
- Pain or tenderness
- Pus or foul-smelling discharge
Systemic Symptoms
- Fever
- Chills
- Fatigue
- Elevated blood sugar levels
Diagnosis of Diabetic Foot Infections
Clinical Examination
Doctors assess wound depth, discharge, odor, and surrounding skin condition.
Laboratory Tests
Blood tests and wound cultures help identify the type of infection.
Imaging Studies
X-rays, MRI, or CT scans detect deep tissue or bone involvement.
Treatment Options for Diabetic Foot Infections
Wound Care and Debridement
Removing dead tissue is like clearing debris from a road—it allows healing to move forward.
Antibiotic Therapy
Oral or IV antibiotics are prescribed based on infection severity and culture results.
Surgical Interventions
Surgery may be needed to drain abscesses or remove infected tissue.
Amputation as a Last Resort
When infection threatens life, amputation becomes necessary. The goal is always limb preservation first.
Advanced Therapies for Diabetic Foot
Negative Pressure Wound Therapy
This technique uses suction to promote faster healing and reduce infection risk.
Growth Factor and Stem Cell Therapy
Advanced regenerative treatments help stimulate tissue repair.
Hyperbaric Oxygen Therapy
High-pressure oxygen boosts healing by increasing oxygen delivery to tissues.
Importance of Glycemic Control
Glycemic control refers to maintaining blood sugar levels within a healthy target range. For people living with diabetes, good glycemic control is essential to prevent both short-term problems and long-term complications. Consistently managing blood glucose levels improves overall health, quality of life, and reduces the risk of serious conditions.
Blood Sugar Management
Good glucose control accelerates healing and reduces infection risk.
Role of Diet and Medication
Balanced meals, insulin, and oral medications work together to protect your feet.
Prevention of Diabetic Foot Infections
Diabetic foot infections are a serious but largely preventable complication of diabetes. High blood sugar levels, nerve damage, and poor blood circulation increase the risk of foot injuries and infections. With proper daily care, early detection, and good diabetes management, most diabetic foot infections can be avoided.
Daily Foot Care Routine
- Inspect feet daily
- Wash and dry thoroughly
- Moisturize (avoid between toes)
Proper Footwear Selection
Choose cushioned, well-fitted shoes and diabetic socks.
Regular Medical Checkups
Routine foot exams catch problems early—before they explode into emergencies.
Complications of Untreated Diabetic Foot Infections
Diabetic foot infections are a serious complication of diabetes. When left untreated or inadequately treated, these infections can progress rapidly and lead to severe, sometimes life-threatening outcomes. Below are the major complications associated with untreated diabetic foot infections, explained clearly for better understanding.
Gangrene
Severe infection combined with poor blood supply can lead to tissue death, known as gangrene. The affected area may turn black or dark and emit a foul odor. Gangrene is a medical emergency.Tissue death due to poor blood supply and infection.
Sepsis
If bacteria enter the bloodstream, the infection can spread throughout the body, leading to sepsis. This life-threatening condition can cause organ failure, shock, and death if not treated immediately.A life-threatening condition where infection spreads to the bloodstream.
Limb Loss
Amputation affects mobility, mental health, and quality of life.
Living With Diabetes: Protecting Your Feet
Living with diabetes requires daily care and attention, and foot health is one of the most important aspects often overlooked. High blood sugar levels can damage nerves and blood vessels, increasing the risk of foot problems such as infections, ulcers, and even amputations. With proper knowledge and routine care, most diabetic foot complications can be prevented.
Lifestyle Modifications
Quit smoking, exercise regularly, and maintain a healthy weight.
Patient Education and Awareness
Knowledge is power. Understanding warning signs can save your foot—and your life.
Conclusion
Diabetic foot infections may start small, but their consequences can be enormous. The feet quietly carry us through life—ignoring them is a costly mistake. With proper blood sugar control, daily foot care, timely medical attention, and awareness, diabetic foot infections can be prevented or treated successfully. Remember, when it comes to diabetic feet, early action isn’t just smart—it’s lifesaving.
FAQs
1. Can diabetic foot infections heal completely?
Yes, with early diagnosis, proper treatment, and good blood sugar control, most infections heal well.
2. How often should diabetics check their feet?
Daily self-examination is recommended, along with regular doctor visits.
3. Are antibiotics always required?
Most infections need antibiotics, but the type and duration depend on severity.
4. Can home remedies treat diabetic foot infections?
No. Home remedies may worsen the condition. Medical care is essential.
5. What is the biggest risk factor for amputation?
Delayed treatment and uncontrolled blood sugar levels.


