Introduction to Diabetic Foot Problems
Diabetes requires you to take as much care of your feet as you do of your blood sugar. As a physician, I’ve seen hundreds of patients who arrive with minor symptoms like burning, numbness, or a small wound, and within weeks, they experience avoidable complications. This blog describes the specifics of how diabetic foot issues arise, how medical professionals handle them, and what you can do to maintain your health, safety, and mobility.
Why Diabetic Foot Needs Expert Attention
Diabetic foot is a medical emergency waiting to happen, not just a wound. The majority of patients arrive believing they have “just a small cut,” but in reality, even minor wounds can develop into infections in a matter of hours. As a physician, I’ve witnessed innumerable instances where prompt medical intervention could have prevented suffering, wasted time, and cost.
The Real Reason Diabetic Foot Complications Are Growing
These conditions are rapidly spreading throughout the world due to a number of factors, including a modern lifestyle, poor sugar control, an unhealthy diet, ignorance, and ignoring early foot symptoms.
What Happens in Your Body When Blood Sugar Stays High
Two significant issues arise when blood sugar levels stay elevated for months or years:
damage to the nerves (neuropathy)
decreased blood flow (ischemia)
When combined, they create the conditions for serious foot issues.
How Diabetes Damages the Feet
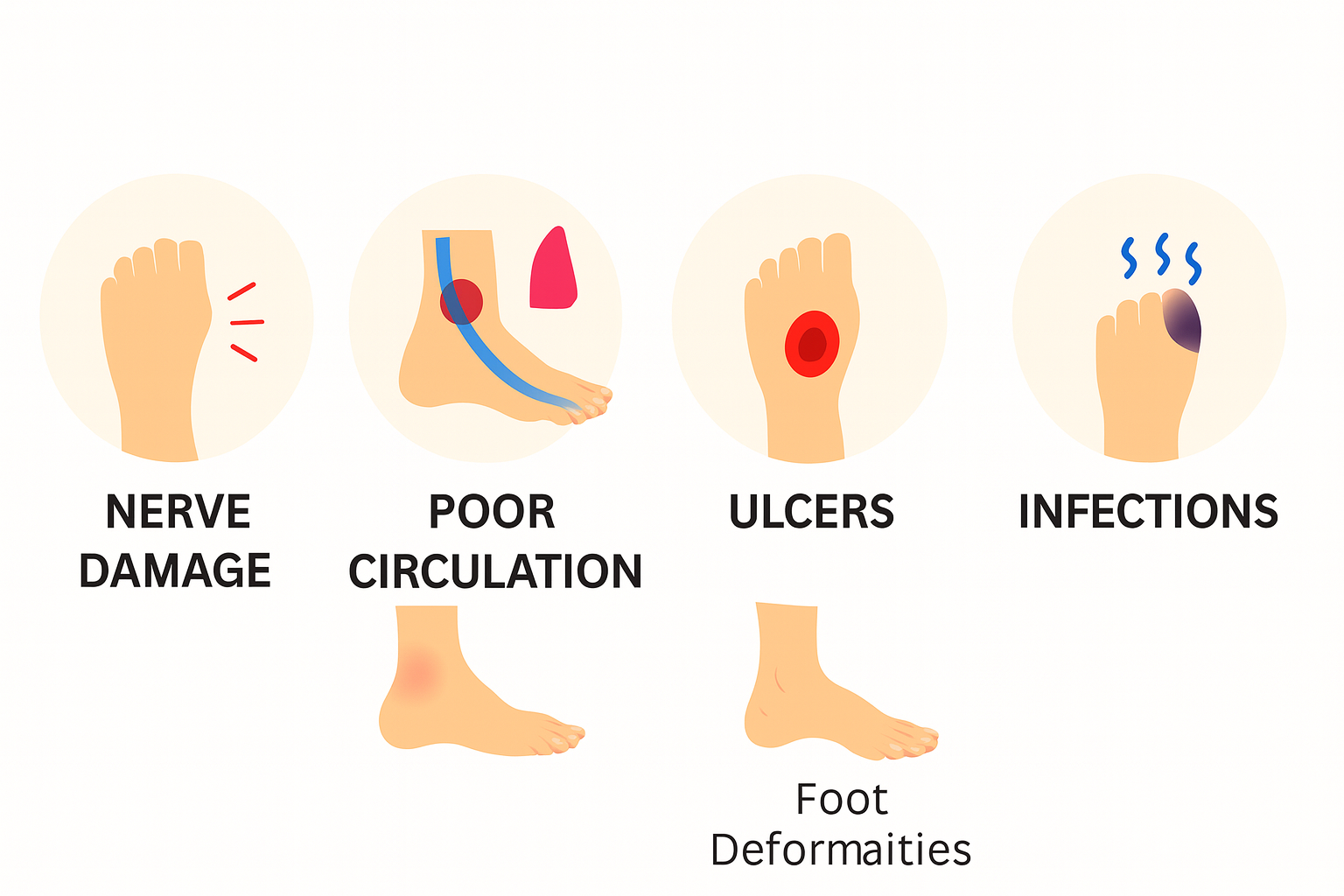
Neuropathy: The Silent Damage
Your capacity to feel is diminished by neuropathy.
- Pain
- Warmth
- The pressure
- Cuts and scrapes
Because of this, diabetic patients frequently fail to notice wounds until they are quite serious.
Poor Blood Circulation
The blood flow to the feet is diminished by peripheral artery disease (PAD). Wounds cannot heal properly if circulation is poor.
Repeated Pressure & Unnoticed Injuries
Wounds beneath the skin are caused by calluses, tight shoes, and uneven walking pressure.
Foot Deformities Over Time
Walking is painful and increases the risk of ulcers if you have claw toes, hammer toes, or Charcot foot deformity.
Early Warning Signs You Should Never Ignore
Numbness & Burning Sensations
A sign of sensory nerve damage.
Skin Texture Changes
Dryness, cracks, and peeling are early indicators.
Slow-Healing Wounds
If a wound doesn’t heal in 7–10 days, it’s a red flag.
Redness, Swelling & Local Warmth
These often mean infection is beginning.
Types of Diabetic Foot Conditions
Neuropathic Ulcers
caused by pressure points and loss of feeling.
Ischemic Ulcers
Caused by poor blood flow—typically painful.
Neuro-ischemic Ulcers
Ischemia plus neuropathy is a dangerous combination that increases the risk of infection and slows healing.
Cellulitis & Deep Tissue Infections
infection of soft tissues that spreads beneath the skin.
Osteomyelitis
Bone infections are extremely challenging to cure and necessitate long-term antibiotic use.
Gangrene
dead tissue as a result of inadequate blood flow. a medical emergency that needs to be treated right away.
How Doctors Diagnose Diabetic Foot Problems Thoroughly
Neurological Examination
We check:
- Feeling
- The vibration
- Reflexes
- Reaction to pressure
Vascular Evaluation
Using:
- Doppler
- ABI
- Pressure on the toes
- Checking the pulse
Wound Depth & Classification
Doctors measure:
- Dimensions
- Depth
- The existence of pus
- Bone exposed
- Damage to tissue
Advanced Imaging
- X-ray: bone infection
- MRI: deep abscesses
- CT scan: deformities
Blood Tests & Culture Tests
Identify infection-causing bacteria to select the right antibiotics.
Medical Treatments Doctors Use to Cure Diabetic Foot
Wound Debridement
Healing is impeded by dead tissue. A clean wound bed is produced by debridement.
Pressure Offloading Techniques
Physicians utilize:
- Complete contact casting
- Shoes for diabetics
- Personalized insoles
- Walkers with orthopaedics
Antibiotics & Infection Control
According to cultural reports, physicians recommend:
- Antibiotics taken orally
- For severe cases, intravenous antibiotics
Blood Flow Restoration Procedures
Angioplasty or bypass surgery is advised if blocked arteries impair blood flow.
Treating Underlying Conditions
Controlling:
- Blood sugar
- BP
- Cholesterol
- Kidney function
helps healing faster
Advanced and Modern Diabetic Foot Treatments
PRP & Growth Factor Therapy
Uses platelets to accelerate wound healing naturally.
Stem Cell Therapy
encourages the healing and regeneration of tissue.
Hyperbaric Oxygen Therapy
In a pressurized chamber, patients breathe 100% oxygen. improves oxygen delivery and circulation.
Negative Pressure Wound Therapy (NPWT)
A vacuum machine that removes wound fluid, increases blood flow, and promotes quick healing.
Bioengineered Skin Substitutes
Wounds are covered by artificial skin layers, which hasten the healing process.
Surgical Options for Severe Cases
Drainage & Cleaning of Deep Infections
eliminates contaminated tissues and pus.
Correction of Foot Deformities
lowers the risk of ulcer recurrence.
Revascularization Surgery
restores blood flow in order to stop tissue death.
Amputation
only carried out when an infection poses a serious risk to life.
Long-Term Management & Preventive Care
Daily Home Care Routine
- Examine your feet every day
- Hydrate
- Carefully clean your nails
- Don’t go barefoot
Footwear & Offloading
Wear:
- Soft soles:
- Shoes for Diabetics
- Shoes that relieve pressure
Blood Sugar Management
essential for the healing of wounds.
Regular Follow-Ups With Specialists
Visit every 1–3 months.
Doctor’s Expert Tips for Fast Healing
Diet That Helps Wound Healing
Include:
- The protein
- Vitamin C
- Zinc
- Fatty acids with omega-3
Exercises to Improve Blood Circulation
- Walking
- Toe stretches
- Ankle rotations
Lifestyle Habits That Save Your Feet
- Quit smoking
- Manage stress
- Maintain healthy weight
Conclusion
Despite its seriousness, diabetic foot is completely treatable with the correct medical attention, prompt diagnosis, and a solid preventative strategy. As physicians, our goals extend beyond treating ulcers to include saving limbs and improving quality of life. The majority of patients can recover completely with today’s sophisticated treatment options if they take prompt action and adhere to their doctor’s advice.
FAQs
1. Is it possible to cure diabetic foot completely?
Yes, ulcers can heal entirely if they are identified early and treated appropriately.
2. How quickly can a diabetic foot ulcer be healed?
Debridement, offloading, sugar regulation, and infection control.
3. What causes the slow healing of diabetic wounds?
Healing is delayed by poor blood flow, nerve damage, and elevated blood sugar.
4. Is it possible to walk while having a diabetic foot ulcer?
Walking raises the pressure, so it’s important to offload.
5. When ought I to visit a physician?
whenever numbness, redness, swelling, or slowly healing wounds appear.


