
Introduction
Prevention, Symptoms & Treatment Living with diabetes is more than just keeping your blood sugar in check—it affects nearly every organ in your body, including your feet. As a doctor, I often see patients walk into my clinic with minor foot issues that could have been easily prevented, only to find they have developed into severe complications. Diabetic foot care is not a luxury; it’s a necessity that can save your mobility, independence, and even your life.
What is Diabetic Foot?
The two main causes of diabetic foot, a dangerous consequence of diabetes, are insufficient blood circulation and neuropathy, or damage to the nerves. These underlying problems make the feet more vulnerable to infections and other ailments. These vulnerabilities may cause wounds to heal more slowly, which might make pre-existing issues worse. These issues might worsen into more serious ailments like ulcers if treatment is not received. In extreme situations, gangrene may result from the extent of the damage, greatly raising the possibility that an amputation may be necessary. Therefore, in order to stop diabetic foot issues from getting worse, prompt intervention and efficient management are essential.
Why Diabetic Foot Care is Crucial
Blood arteries and nerves are silently harmed by high blood sugar. You lose your sense of pain, heat, or injury in your feet when your nerves are injured. This implies that a minor cut or blister may go unnoticed and eventually worsen into a major wound. Infections can spread swiftly and healing is further slowed by poor circulation. One of the main reasons diabetes people are admitted to hospitals is diabetic foot ulcers, according to the World Health Organization.
Symptoms of Diabetic Foot
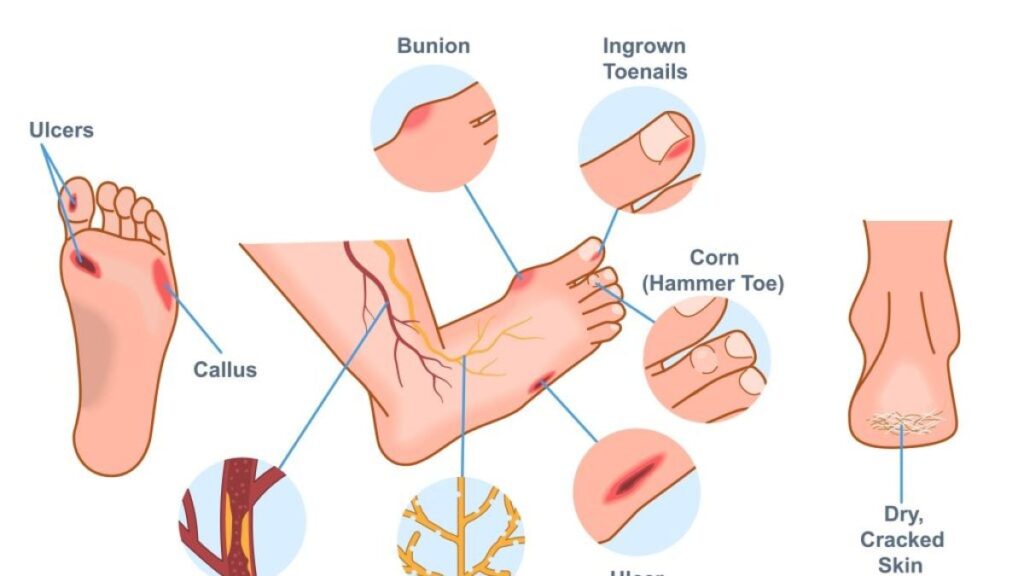
Early Signs
- Burning or tingling in the feet
- Sensation loss (numbness)
- Redness or swelling around the foot
- Dry or cracked skin
Severe Symptoms
- Open wounds that refuse to go away
- Pus, an unpleasant smell, or gangrene-blackened skin
- Abrupt loss of feeling or excruciating agony
When to See a Doctor
See your doctor right away if you observe any changes in skin color, fever, spreading redness, or wounds that don’t heal in two weeks. Treatment delays may lead to serious infections or even amputation.
Risk Factors for Developing Diabetic Foot
- Over time, poor blood sugar regulation
- Smoking (decreases blood flow)
- Overindulgence in drinking (increases neuropathy)
- Donning shoes that are too tight or poorly fitted
- History of foot injuries or ulcers
Prevention of Diabetic Foot Complications
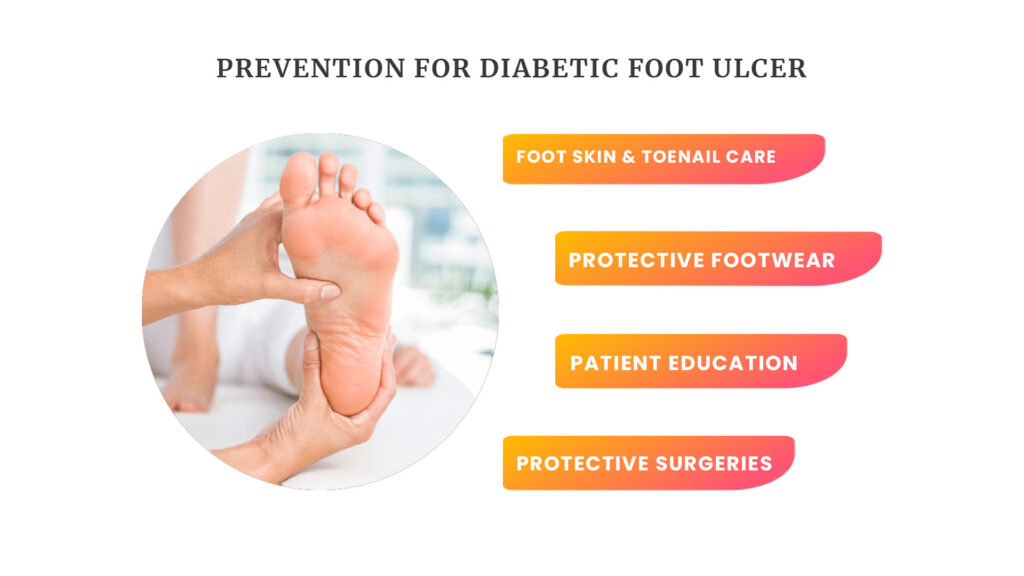
Daily Foot Inspection
Ask a family member or use a mirror to examine your feet each day. Keep an eye out for any wounds, blisters, swelling, or skin color changes.
Proper Hygiene and Nail Care
Keep your toenails clipped straight, wash your feet every day with lukewarm water, and dry them completely, paying specific attention to the spaces between your toes.
Choosing the Right Footwear
Put on well-fitting, closed, cushioned shoes. Even at home, don’t go barefoot.
Controlling Blood Sugar and Lifestyle Changes
Exercise, stopping smoking, and maintaining a healthy blood sugar level all greatly enhance circulation and reduce risk.
Medical Diagnosis of Diabetic Foot Problems
To assess for circulation and neuropathy, doctors typically do a clinical examination. While imaging procedures (MRI, X-ray) look for bone involvement, blood tests can detect infections. Some clinics evaluate the health of the blood vessels and nerves using doppler ultrasonography or monofilament tests.
Treatment Options for Diabetic Foot
Non-Surgical Treatments
- Particular treatments that assist the healing of wet wounds
- Using antibiotics to prevent infections
- Offloading tools (specific footwear or pressure-relieving casts)
Surgical Treatments
- Debridement: removing tissue that has died
- Grafts of skin: for big ulcers
- Amputation: in dire circumstances to preserve life
Advanced Therapies
Treatments including negative pressure wound therapy, hyperbaric oxygen therapy, and even stem cell-based therapies are showing encouraging outcomes.
Role of a Multidisciplinary Team
It takes more than one doctor to treat diabetic foot disease. Nurses, podiatrists, vascular surgeons, wound care specialists, and endocrinologists are all involved. Cooperation guarantees greater results and quicker healing.
Home Care Tips for Diabetic Foot Patients

- Every day, wash, moisturize, and check your feet.
- Steer clear of hot water or heating pads as they increase the risk of burns from numbness.
- Inform your physician right once of any wounds, no matter how small.
Lifestyle Modifications for Better Foot Health
Healthy feet are a result of a balanced diet, consistent exercise, and stopping smoking. Simple exercises like walking can increase blood flow. Controlling stress also indirectly aids with blood sugar regulation.
Myths vs. Facts About Diabetic Foot
- Myth: It’s excellent to soak your feet every day.
- Fact: Dangerous infections can develop from even minor wounds.
- Myth: If you have diabetes, small cuts don’t matter.
- Fact: Extended soaking can lead to skin dryness and cracking.
- Myth: Amputation is always the result of diabetic foot.
- Fact: Most instances can be resolved without surgery if care is received early.
Psychological Impact of Diabetic Foot
Anxiety and despair might result from having ongoing wounds or from being afraid of being amputated. In order to rehabilitate and cope, family support, counseling, and support groups are essential.
Future of Diabetic Foot Care
Wearable foot pressure monitoring devices, and novel regenerative therapies all bode well for the future. To find issues before symptoms show up, early detection methods are being created.
Conclusion
The key to diabetic foot care is being vigilant, preventing, and seeking medical help as soon as possible. “Your feet carry you through life, don’t let diabetes take them away,” I advise my patients as a doctor. The majority of foot issues are preventable or easily treatable with the correct information and frequent attention. Never forget that prevention is always preferable to treatment.
FAQS
1. Is it possible to entirely avoid diabetic foot?
Yes, the majority of diabetic foot issues may be avoided with careful blood sugar management, frequent foot exams, and appropriate footwear.
2. What are the finest shoes for people with diabetes?
The ideal shoes are closed, cushioned, soft, and well-fitting. Don’t wear sandals, slippers, or go barefoot.
3. How frequently should a person with diabetes examine their feet?
Self-checks are crucial every day. Additionally, at least once a year, have your feet examined by your physician.
4. Are natural solutions for diabetic foot care safe?
No, a lot of home cures might make the illness worse. For any cut or infection, always get medical advice.
5. What part does nutrition play in preventing diabetic foot disease?
A nutritious diet lowers the incidence of foot problems by promoting circulation, reducing inflammation, and assisting in blood sugar regulation.


