Introduction
Diabetes is a disorder that can gradually harm blood vessels and nerves; it’s not just high blood sugar. Diabetic foot is one of its most dangerous side effects, which can result in amputation if left untreated. As a physician, I have seen firsthand the anguish of losing a limb as well as the satisfaction that comes from saving a limb through early intervention. This blog seeks to inform patients and caregivers about the causes, prevention, and recovery process of diabetic foot amputation.
Understanding Diabetic Foot
Diabetic foot: What is it?
Uncontrolled diabetes causes poor circulation and nerve damage (neuropathy), which results in wounds or ulcers that heal slowly. This condition is known as diabetic foot. Infections can spread quickly if treatment is delayed.
The Impact of Diabetes on Nerves and Circulation
Elevated glucose damages tiny blood vessels, which lowers the amount of oxygen and nutrients that reach the tissues. Patients may not notice a cut or blister until it becomes infected because damaged nerves result in numbness.
Typical Warning Indications
- Tingling or numbness
- Redness or swelling
- wounds that don’t heal
- offensive-smelling discharge
Complications can frequently be avoided by recognizing these symptoms early.
Causes Leading to Amputation

Amputation is typically the last option when all other therapies have failed, so it is not a quick fix. Among the primary causes are:
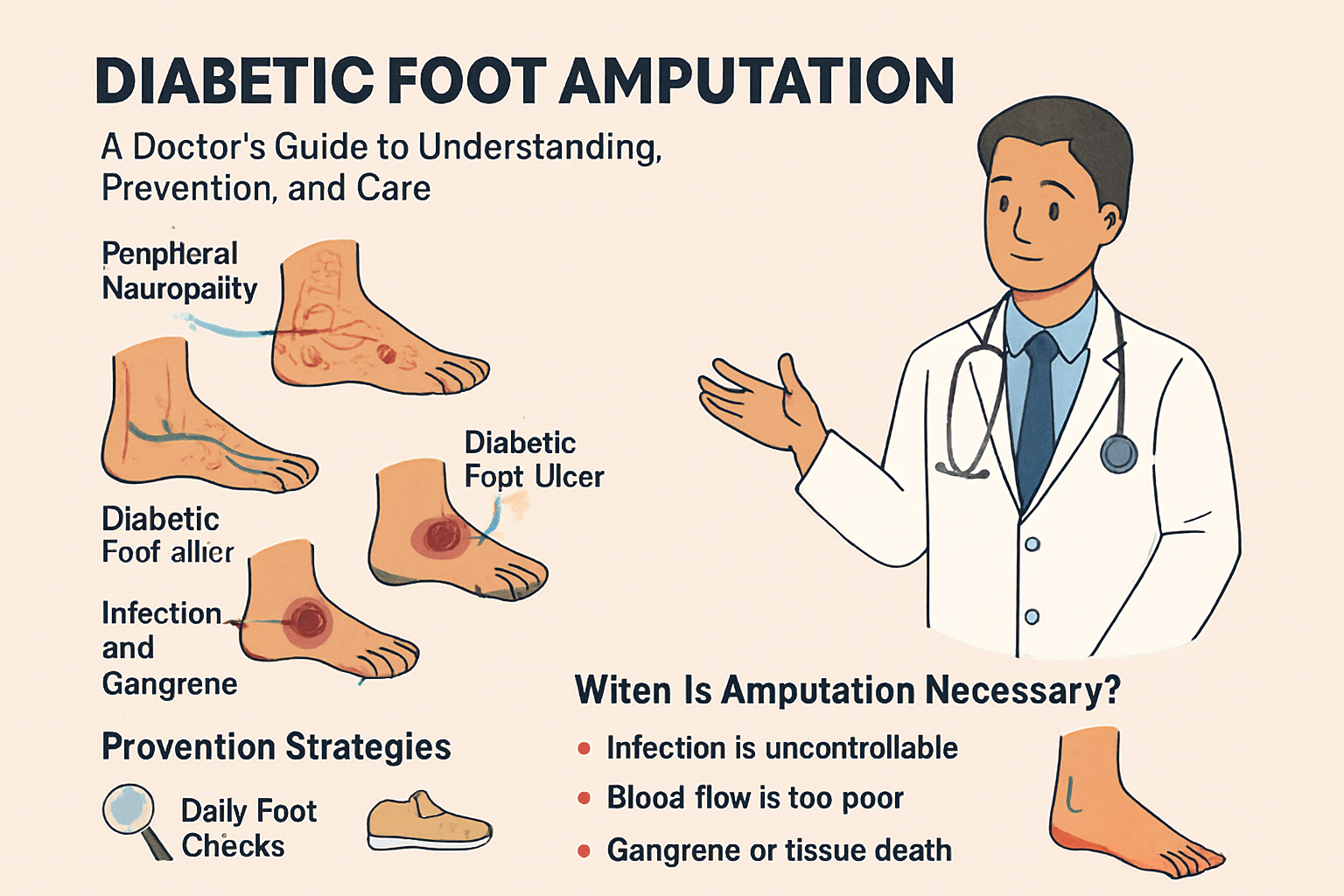
Neuropathy in the Periphery
Damage goes unnoticed when there is a loss of feeling. Small cuts have the potential to grow into large, infected ulcers.
Inadequate Blood Flow (Peripheral Artery Disease)
Reduced blood flow raises the risk of infection and hinders healing.
Ulcers and Infections
Amputation may be necessary if bacterial infections (osteomyelitis) spread to the bone.
Ignorance or Postponed Care
Self-treating with home remedies or ignoring wounds frequently makes the condition worse.
When Amputation Becomes Necessary
Warnings
- A potentially fatal infection
- Dead tissue or gangrene
- Bone-related non-healing ulcers
- Uncontrolled sepsis
Amputation Types
- Removing one or more toes is known as toe amputation.
- Transmetatarsal Amputation: This procedure keeps the heel intact while removing a portion of the foot.
- When an infection spreads past the ankle, below-knee amputation (BKA) is performed.
- A rare procedure used when circulation to the lower leg is severely compromised is above-knee amputation (AKA).
Pre-Amputation Evaluation
Before surgery, physicians conduct a number of tests:
- Angiography or Doppler: To measure blood flow
- MRI or X-rays: To identify bone infections
- Blood tests: To assess infection indicators and sugar regulation
Vascular surgery is attempted whenever possible in an effort to restore blood flow and prevent amputation.
Surgical Approach
Deciding on the Level
The goal of surgery is to remove the diseased tissue while maintaining optimal function. The degree of infection and circulation quality determine the extent of amputation.
The process
Under anesthesia, healthy margins are maintained while dead tissue is removed. Infection is managed with drainage and antibiotics.
Measures for Safety
To guarantee a speedy recovery, strict sterilization, glucose control, and antibiotic coverage are upheld.
Postoperative Care
Amputation-related healing is a delicate process.
Management of Wounds
Using sterile methods, dressings are changed on a regular basis.
Control of Infections
Depending on the culture results, broad-spectrum antibiotics are administered.
Control of Glycemic
Blood sugar stability encourages quicker recovery and guards against reinfection.
Recovery After Amputation
Stay in the Hospital
Depending on their rate of recovery, patients typically stay in the hospital for 7–14 days.
Pain Control
Patients are kept comfortable by contemporary painkillers and blocks.
Rehabilitation
Maintaining muscle strength and mobility is aided by early physiotherapy.
Psychological Support
Through counseling, patients can regain their confidence and make emotional adjustments.
Prosthetics and Mobility
Prosthetics, or artificial limbs, enable movement that is almost normal thanks to modern technology.
- Custom prosthetics enhance functionality and comfort.
- Adapting to new mobility is aided by gait training.
- Frequent examinations guarantee a good fit and avoid skin problems.
Preventing Diabetic Foot Amputation

Foot Care
Use lukewarm water to wash every day.
Keep your feet moisturized and dry.
Wearing the Right Shoes
Put on socks and shoes with cushions.
Don’t go barefoot.
Typical Medical Visits
routine examination for circulation issues and ulcers.
Minor injuries should be treated right away.
The Role of a Doctor in Managing Diabetic Foot
A doctor’s work involves more than just treating patients; it also involves saving lives and limbs.
- multidisciplinary care : Physiotherapists, podiatrists, diabetologists, and surgeons are all involved in multidisciplinary care.
- Patient education : includes instruction in glucose management and foot care.
- Timely Decision-Making : Understanding when to save the limb and when to operate.
Patient Education and Self-Care Tips
- When fasting, keep blood sugar levels below 140 mg/dl.
- Examine your feet every day using a mirror.
- Carefully trim your nails.
- Never disregard minor blisters or cuts.
Real-Life Case Insights
A 58-year-old man with uncontrolled diabetes showed up with toe gangrene. The toe was saved following wound care and vascular intervention. Another instance of below-knee amputation due to delayed consultation serves as a reminder of the significance of prompt medical attention.
Conclusion
Amputation of the diabetic foot is not always necessary; it is frequently avoidable. Many patients can prevent limb loss with proper wound care, frequent checkups, and good blood sugar control. Modern medicine gives those who do have amputations hope for independence and recovery. Keep in mind that your best defense is awareness.
FAQS
1. Is it possible for diabetic foot to heal without amputation?
Yes, amputation can be avoided with appropriate wound care and infection control if caught early.
2. How can I determine the severity of my foot infection?
Keep an eye out for pus, swelling, a bad odor, or spreading redness—all of which require immediate medical attention.
3. Does using a prosthetic hurt after being amputated?
It requires some getting used to at first, but with proper physiotherapy, it becomes comfortable.
4. How much time does it take to heal from an amputation?
6–12 weeks on average, depending on recovery, sugar management, and health.
5. Is it possible to totally avoid amputations?
Yes, in the majority of cases—with early intervention, appropriate footwear, and routine monitoring.


