Introduction
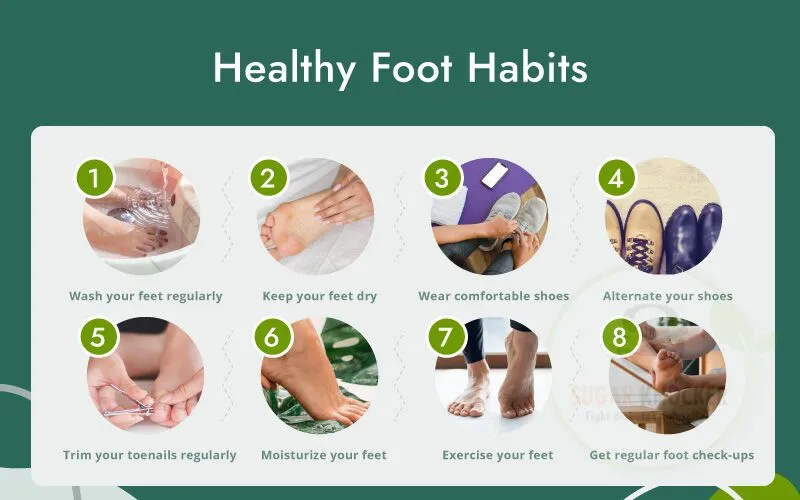
Daily Foot Care Routine You have to be mindful of every part of your body when you have diabetes, and your feet need special attention. As a physician, I constantly remind my patients that, with the correct daily routine, the majority of diabetic foot issues are avoidable. Imagine treating your feet with the same respect that you give to checking your blood sugar or brushing your teeth. Your feet require more care than you may realize if you have diabetes. Why? Due to diabetes’s effects on nerve sensitivity and blood circulation, you might not become aware of an injury until it’s too late. As a physician, I have witnessed numerous patients experience serious consequences from minor issues like blisters.
Understanding Diabetes and Foot Health
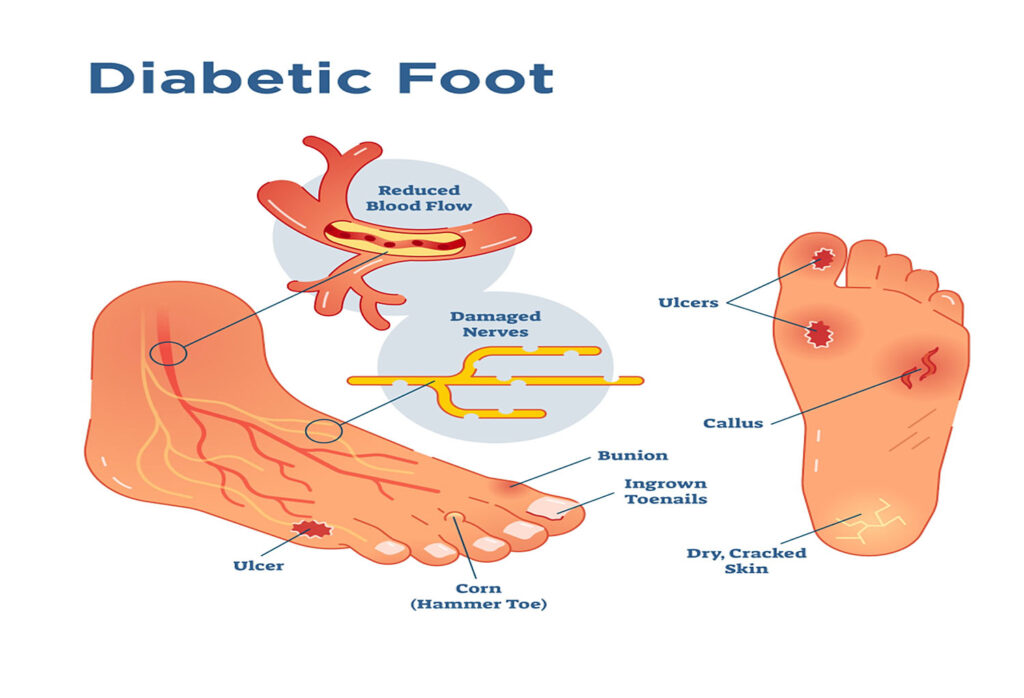
Diabetes can limit blood flow and cause neuropathy, or damage to the nerves. This facilitates the spread of infections and hinders the healing of wounds. If left untreated, even a minor blister can develop into a dangerous ulcer. Because of this, diabetic foot care is more about prevention than cure.
Diabetes impacts your body in two major ways:
- Nerve damage that impairs foot sensation is known as peripheral neuropathy.
- Peripheral artery disease, or poor circulation, slows healing because there is less blood flow.
These make for a dangerous combination. A minor cut might not hurt, but because of the restricted blood flow, it heals poorly, which allows an infection to enter. If left untreated, this may eventually result in gangrene, ulcers, and even amputations.
Common foot problems in diabetic patients
- Cracks and dry skin
- Calluses and blisters
- Fungal infections (nail fungus, athlete’s foot)
- Wounds that don’t heal and ulcers
- Toenail ingrown
The Importance of a Daily Foot Care Routine
Why every day? Because things can change in an instant. Due to nerve damage, a small cut might not hurt, but it could get worse very fast. You can avoid serious consequences, such as amputations, by practicing basic foot care for 10 to 15 minutes each day.
- Because ulcers are costly, painful, and dangerous, prevention is preferable to treatment.
- Being inconsistent is important because even a few days off can put you in danger.
- You take charge of your own health when you are empowered.
Step 1: Daily Foot Inspection
Spend a few minutes each evening checking your feet:
- Keep an eye out for any cuts, cracks, swelling, or changes in color.
- For the soles, use a mirror or enlist the assistance of a family member.
- Blisters, ingrown toenails, and redness should not be ignored.
Step 2: Washing Feet Properly
Use mild soap and lukewarm water to wash your feet. You may not be aware that hot water is burning your skin because it damages your nerves. Don’t scrub too hard, but gently clean between your toes.
Sweat, bacteria, and dirt that can lead to infections are eliminated when you wash your feet.
How to do it correctly:
- Make use of lukewarm water and test with your elbow rather than your foot.
- Select a gentle soap that doesn’t have any scent.
- Wash gently, making sure to get in between your toes.
- Don’t soak your feet for too long because it can cause cracks and dry out the skin.
Step 3: Drying Carefully
Make sure your feet are completely dry, especially in between the toes. The moisture that is trapped there may encourage the growth of fungi. Instead of rubbing firmly, pat with a soft towel.
The enemy of diabetic feet is moisture.
- Instead of rubbing, gently pat dry.
- For toes, use a gentle towel; some patients even use a cool hair dryer setting.
- Make sure the space between your toes is dry.
Step 4: Moisturizing the Right Way
Dry skin, which can crack and become infected, is a common side effect of diabetes. Every day, use a mild moisturizer. However, keep in mind that applying lotion between the toes can cause the area to become overly wet and fungus-prone.
Dry skin is prone to cracking and can serve as a gateway for infections.
- Every day, apply a non-greasy lotion or cream.
- Pay attention to the soles and heels.
- Moisturizing in between the toes raises the risk of fungus.
Step 5: Nail and Callus Care
For diabetics, nail care can be challenging.
- Instead of curving at the edges, trim your nails straight across.
- Use a nail file to smooth out any rough edges.
- Never dig into the sides of your nails or cut the cuticles.
- Consult a podiatrist or your physician if your nails are thick, brittle, or difficult to trim.
Step 6: Choosing the Right Footwear
When it comes to protecting diabetic feet, shoes are crucial.
- Always go for shoes that fit properly and have a wide toe box.
- Steer clear of anything that rubs, such as pointed shoes or high heels.
- Wear new shoes for just one hour at first to break them in.
- If advised, wear diabetic or orthopaedic shoes.
Even indoors, never go barefoot. A tiny stone or needle on the ground could be extremely dangerous.
Step 7: Wearing Protective Socks
In addition to being comfortable, socks also provide injury protection
- Make use of seamless, padded diabetic socks.
- Socks made of cotton or bamboo are breathable and absorb less moisture.
- Steer clear of tight elastic bands that restrict blood flow.
- To stay hygienic, change your socks every day.
Step 8: Managing Corns and Calluses
Avoid the temptation to use store-bought medicated pads or cut corns. Your skin may get burned by these. See a podiatrist instead, who can remove them risk-free.
Avoid using do-it-yourself remedies. Acids found in over-the-counter pads have the potential to harm your skin. Rather:
- For safe removal, see your podiatrist or doctor.
- After bathing, use pumice stones very gently, but only with your doctor’s permission.
Step 9: Monitoring Circulation and Sensation
How to check at home:
- If it takes more than two seconds for your toenail to turn pink again after pressing it, your circulation may be lacking.
- Can you feel it when you run a cotton ball or feather across your foot? If not, neuropathy might be getting worse.
- Inform your physician if you experience cramps, burning, tingling, or numbness.
Step 10: Lifestyle Support for Healthy Feet
Foot care encompasses both your general health and your external activities.
- Control Blood sugar: regulation maintains the health of blood vessels and nerves.
- Eat Well: healthily by consuming foods high in fiber, vitamin C, and omega-3 fatty acids.
- Exercise: Circulation is improved by walking, cycling, or foot stretches.
- Give up smoking: Smoking slows healing and deteriorates circulation.
When to Seek Medical Help
Contact your doctor immediately if you notice:
- After three to four days, wounds are still not healing.
- Redness emanating from a blister or cut
- Thick green or yellow pus
- A sign of gangrene is blackened skin.
- Excruciating foot pain or unexpected edema
Doctor’s Advice: A Preventive Approach
I tell my patients the following:
- Make taking care of your feet a habit rather than a chore.
- Get a professional foot examination from your doctor every three to six months.
- Small changes are frequently early warning indicators, so don’t ignore them.
- Family members can assist with the inspection or serve as a reminder.
Conclusion
You walk through life on your feet; don’t let diabetes take that away. You can maintain your independence, avoid serious complications, and keep your feet healthy with just ten minutes a day. As a physician, I have witnessed the transformative power of seemingly insignificant daily routines.
FAQS
1. Is it appropriate for diabetics to go barefoot at home?
No. Sharp objects can cause minor wounds that go unnoticed and rapidly worsen.
2. Can people with diabetes benefit from foot massages?
Yes, a light massage helps circulation, but if you have ulcers or neuropathy, stay away from deep pressure.
3. Can people with diabetes take warm foot baths?
Sure, but stay away from hot water. Always use your hand or elbow to take the temperature first.
4. Are medicated corn plasters safe?
No. They contain acids that can burn diabetic skin. Always consult your doctor.
5. How can fungal infections be avoided?
Avoid sharing shoes, keep your feet dry, change your socks every day, and apply antifungal powder if necessary.
6. How frequently should I get my feet examined by a doctor?
At least once every six months, or more frequently if you already have foot issues.
7. Can I treat cold feet with heating pads?
No. They can cause skin burns without you noticing. Instead, put on some warm socks.
8. Do diabetic shoes actually have an impact?
Indeed, they protect against injuries and relieve pressure points, particularly in those with neuropathy.


